Why set up a transfer network?
All health providers are required to identify and develop processes that maximise the appropriate use and minimise the wastage of blood and blood products in line with the statement on National Stewardship Expectations for the Supply of Blood and Blood Products1 issued by the Australian Health Ministers.
Implementing a blood and blood product transfer agreement can assist laboratories to:
- enhance the availability of blood and blood product
- manage a limited resource
- reduce unnecessary wastage by transferring blood and blood product to a health provider where it is more likely to be used appropriately.
What do you need to consider?
Identify possible participating transfer health providers
Consider the following factors:
- Other health providers with whom you could set up a transfer arrangement. This could include the following:
- health providers you currently have informal arrangements with;
- health providers located in your local area that you can approach to set up a transfer arrangement;
- health providers within your organisation located in other suburbs or health networks.
- A larger laboratory or health provider that you could transfer your product to, to enhance the possibility of its use before expiry.
- Larger health providers service a varied patient group and are more likely to utilise a range of products before expiry.
- If you are a large laboratory or health provider consider receiving transfers from smaller facilities to enhance the possibility product is used before expiry.
- As a large laboratory or health provider you are more likely to utilise a product before expiry. You could consider reducing your usual order depending on the amount of product you are aware will be transferred in.
- You will need to continually consider the impact on your inventory levels and whether or not you can use the transferred product.
- If you are a smaller laboratory consider reviewing your current inventory if frequent transfers are required.
- If you have an established hub and spoke arrangement consider including other health providers outside these arrangements or your organisation.
- For example, a public local health network hub and spoke could include smaller private health providers in the local area.
- Alternatively, you could consider becoming a hub if you are a large laboratory with a high blood and blood product turnover. This will allow you to manage your own inventory and that of smaller regional facilities with a low turnover. In turn, smaller sites can operate with a lower inventory and still maximise blood use before expiry.
- The proximity of the other health providers to your site.
- Proximity will factor into transport or courier costs and have an effect on validated shipper configuration requirements. Data loggers are currently recommended for all shipments beyond the Blood Service validated transport times when using their shippers.10
- Great distance does not mean a transfer arrangement is not possible. A number of local health networks have transfer or hub and spoke arrangements between a large metropolitan laboratory and smaller regional and remote sites. Examples include Hunter Area Pathology Service in NSW, BloodMove South Australia and Pathology Queensland. For more information see the NBA website at www.blood.gov.au/case-studies.
- Transfer arrangement between public and private health providers.
- Transfer arrangements can work with health providers from different organisations, local health networks, pathology organisations and across the public and private health sectors. BloodMove in South Australia is an example where there is a formal arrangement to transfer blood and blood product between public and private health providers.
- Public health providers who work with a devolved blood budget may wish to discuss the impact of a transfer agreement with the relevant manager of blood budgets within their jurisdiction.
- Suitable options could include exchange of supply with short for long expiry and using existing courier networks. Any issues that may arise with these (or any other proposed options) should be considered, agreed and documented by all parties.
- Transfers between National Association of Testing Authorities (NATA) accredited health providers with blood fridges that are compliant with AS3864 Medical refrigeration equipment – For the storage of blood and blood products6 are relatively easy to set up and should provide assurance that blood and blood products are maintained within manufacturer’s temperature specifications.
Accreditation
Participating health providers are responsible for maintaining the necessary accreditation, standards and legislation (for example as outlined by NATA or Standard 7). This should provide assurance to receiving health providers that any transferred blood and blood products they receive have been stored appropriately. Include a point in your MOU outlining responsibilities of all parties if accreditation requirements are not met.
Review inventory management practice at participating providers
It is recommended that health providers review the current inventory management practice with each product at each laboratory or site participating in the MOU. 10 Tips to Help Manage Your Blood Product Inventory located within Managing Blood and Blood Product Inventory can provide practical advice to appropriately manage blood and blood product inventory.
Review transport options and practices at participating health providers
Review existing blood courier system
Determine if there is an existing courier service you could utilise. If so, investigate the cost to use this service. If not, investigate courier or taxi options and discuss with management to determine the division of costs.
When taking transport into consideration a cost benefit analysis can be undertaken to understand the workload and financial cost of transferring blood and blood products in and out versus the financial cost and loss of a valuable resource. If the cost of transport outweighs the cost of the blood product/s then it may not be feasible to develop regular transfer arrangements in exceptional circumstances.
All signatories on the MOU may invest in a transport option to reduce costs. Examples of transport options include:
- using an existing health provider courier service;
- engaging hire cars, buses or taxis;
- investigating a courier service that specialises in cold product transfer. This may be especially useful for longer distances and flights.
You may consider entering into a Service Level Agreement with your chosen courier company.
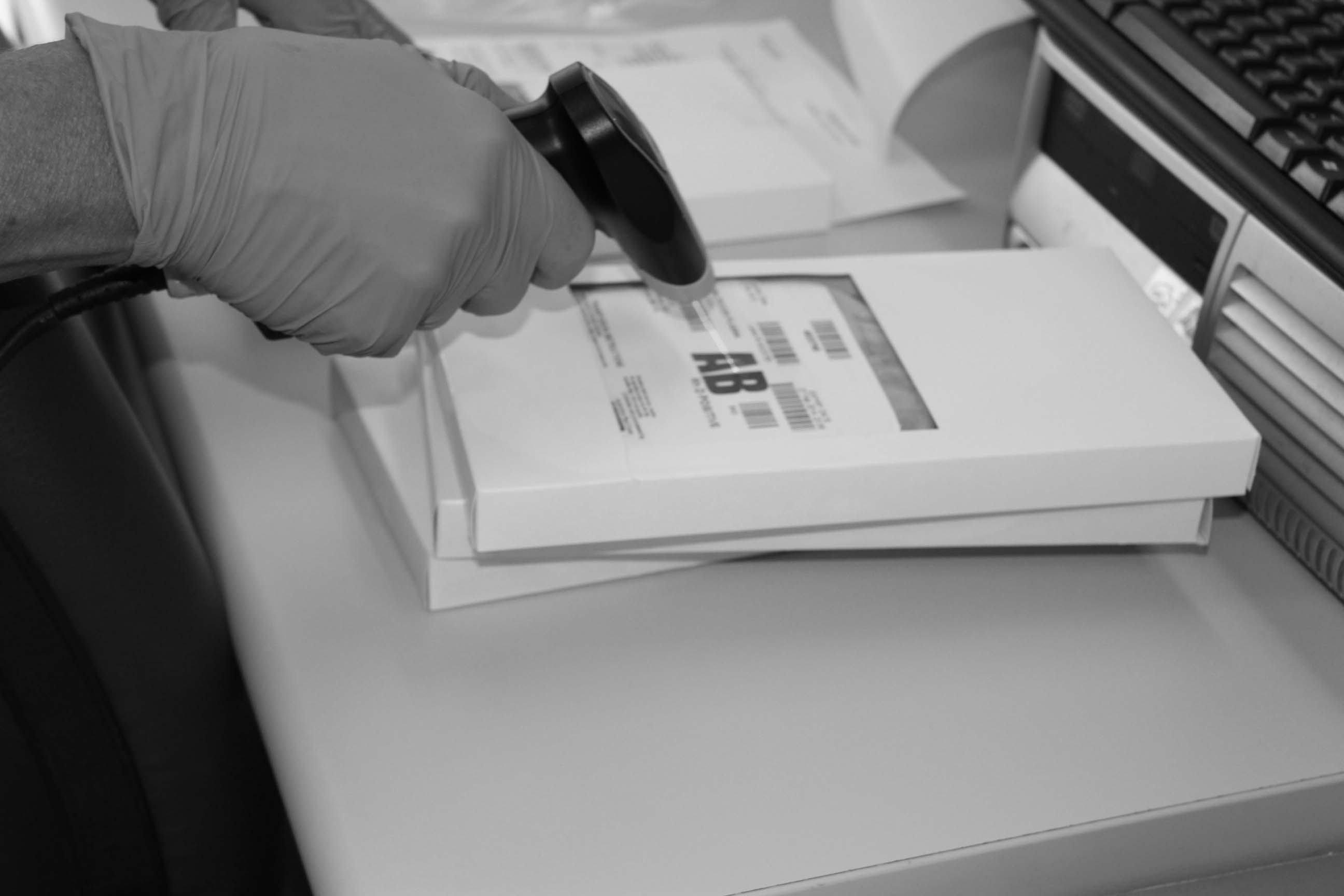
Review existing shipping configuration for the transfer of blood and blood products
In accordance with the National Pathology Accreditation Advisory Council blood and blood products must be transported in validated shipping containers.7 It is important to review what shipping configurations and containers, if any, are currently in use with each health provider participating in the MOU. More information on packing and transport shippers can be found under Packing Requirements, section below.
See Appendix 1: Transfer arrangement checklist for a summary of items to consider when setting up formal transfer arrangements.
See Appendix 2: Example Validation Process for an outline of a possible shipper configuration and validation process.
Next page: Managing Blood and Blood Product Transfers - Implementation
Previous page: Managing Blood and Blood Product Transfers - Scope and Introduction

